By Marc J. Fine, MPH
Background:
Abdominal aortic aneurysms (AAAs) are found in more than 5% of patients over 50 years of age, and cause 15,000 deaths/year in the United States. The mortality of AAA rupture is up to 90%. Though most intact aortic aneurysms do not produce symptoms, the diagnosis of an abdominal aortic aneurysm can be confirmed by the use of ultrasound. The exam is rapid, non-invasive, and easy to perform. Medicare and other insurance typically reimburse for this exam.
Procedure:
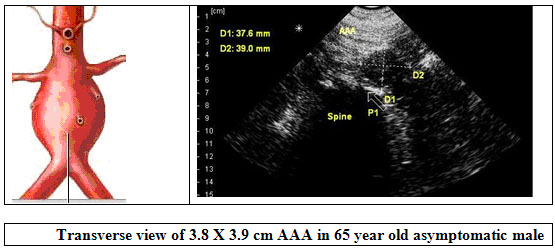
A series of distance measurements is made in the longitudinal and transverse planes of the aorta, from the level of the xyphoid down to the point of bifurcation — from outer wall to outer wall of the aorta. The normal aorta measures 3 cm. or less. If the outer diameter of the abdominal aorta is greater than 3 cm, the patient should be referred for workup and evaluation. A diameter greater than 5 cm is associated with an increased risk of rupture.
Conclusion:
Patients today aren’t routinely screened for AAA because of the inconvenience and cost of referral to a diagnostic imaging center. Ultrasound is now trickling down to primary care providers and many believe it will soon be a standard of care during the routine physical exam, much as recording blood pressure, auscultation of the heart and lungs, and taking a family history. Other benefits of primary care scanning include: documenting the presence of two kidneys as well as other incidental findings, such as identifying kidney or gall stones, other abdominal masses, pregnancy, bladder volume, etc.
References and Notes
Mayo Clinic Guidelines:
Regular screening for people at risk of abdominal aortic aneurysms. Because aortic aneurysms often don’t cause symptoms, anyone age 60 and older who has risk factors for developing an aortic aneurysm should consider regular screening for the condition. Men ages 65 to 75 who have ever smoked should have a one-time screening for abdominal aortic aneurysm using abdominal ultrasound. Men age 60 and older with a family history of abdominal aortic aneurysm should also consider screening.
Epidemiology:
AAA’s affect 6-9% of men over 65 years of age. They are twice as common in men than in women. The major risk associated with AAA’s is that they have a high propensity to rupture. Ruptured AAA’s are the 13th leading cause of death in the United States. They are also the 10th leading cause of death for men over the age of 55. Approximately 30% to 50% of patients with a ruptured AAA die before they ever reach a hospital. Even with surgery, there is 50-70% mortality rate associated with a ruptured AAA. Therefore, early detection and timely repair are paramount to AAA management. The rate of aneurysm rupture is related to its size. A 4.0 cm AAA has a 1% risk of rupture per year while a 6.0 cm AAA has a 10% risk of rupture per year. Risk factors such as smoking and high blood pressure) may increase the size of the AAA, the rate of growth, and the risk of rupture. (USC School of Medicine)
Creager, MA, Halperin, JL, Whittemore, AD.
Aneurysmal disease of the aorta and its branches. In: Vascular Medicine, Loscalzo, J, Creager, MA, Dzau, VJ (Ed), Little, Brown, New York, 1996, p. 901.
Brown LC, Powell JT
“Risk factors for aneurysm rupture in patients kept under ultrasound surveillance. UK Small Aneurysm Trial Participants.”
U.S. Preventive Services Task Force (2005).
“Screening for abdominal aortic aneurysm: recommendation statement.” Ann. Intern. Med. 142 (3): 198–202.
Video:
“Ultrasound Use In The Diagnosis Of Abdominal Aortic Aneurysm”
Department of Emergency Medicine, Hennepin County Medical Center, Minneapolis, Minnesota, in association with hqmeded.com.
Marc Fine is Director of Marketing for Interson Corporation, a Silicon Valley Based Company that makes the SeeMore USB ultrasound imaging probe.